Zeissig Lab
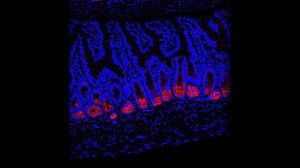
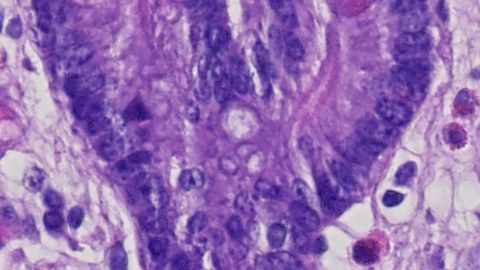
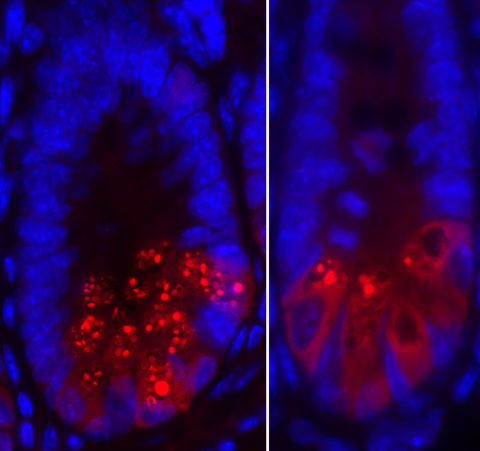
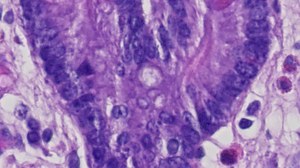
We are interested in the immunological mechanisms which govern homeostasis at mucosal surfaces and the pathways contributing to disruption of homeostasis under conditions of inflammation and tumor development. Our work focuses on the intestine and the liver and associated inflammatory disorders such as inflammatory bowel disease as well as malignant diseases such as colorectal cancer and hepatocellular carcinoma. We are pursuing a translational research strategy combining work in genetically modified mice with studies on human tissues and cells.
 © Zeißig Lab
© Zeißig Lab
Mucosal Immunology
Specific current research topics:
- Immunological alterations and defects in epithelial regeneration in the pathogenesis of inflammatory bowel disease
- Interactions between lipid metabolism, inflammation, and carcinogenesis
- Microbial and immunological regulation of cancer development in the intestine and the liver